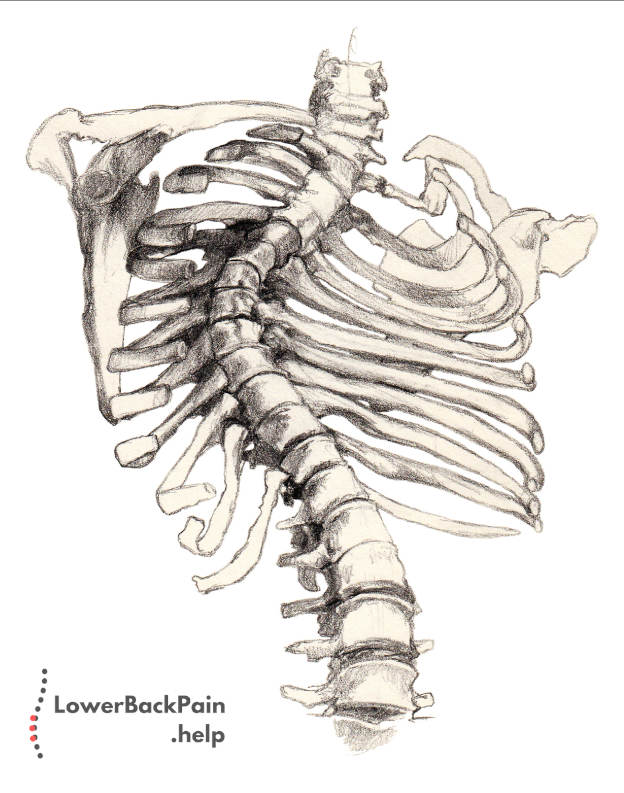
In general, there are three different causes of scoliosis:
- Idiopathic scoliosis. Idiopathic scoliosis develops in adolescence and has no known cause.
- Congenital scoliosis. Congenital scoliosis is caused by genetics and develops before a baby is even born.
- Neuromuscular scoliosis. Neuromuscular scoliosis is caused by another disease, degenerative disorder, or even an injury.
Approximately 65% of scoliosis are idiopathic, 15% are congenital, and 20% are neuromuscular.
Now, let’s take a closer look at each variety of this disorder.
Idiopathic Scoliosis
Idiopathic literally means “of unknown origin”.
In other words, we don’t know where these cases of scoliosis come from, or why they are caused.
We do know that there are genetic factors involved, as well as some environmental factors.
Approximately 1% to 2% of adolescents develop scoliosis, but only about 10 to 20% of cases get worse as the patient grows older.
According to scientists, about 38% of scoliosis risk comes from genetic factors, while 62% of risk comes from the environment.
Environmental factors are well understood.
They include bad posture, heavy backpacks, and sports injuries. The stereotypical “student’s slouch” really is bad for your back!
That said, we’re only beginning to understand the genetic causes of idiopathic scoliosis.
Here’s what we know: Several genes have been associated with scoliosis, including genes related to connective tissue growth, bone growth, and bone metabolism. These genes have been identified by several independent studies of the human genome.
One particular gene, CHD7, has been conclusively linked with scoliosis.
However, just because someone has this gene or even a combination of genes, does not mean they’re automatically going to develop scoliosis.
There are even identical twins, where one twin develops scoliosis and another does not.
This might be due to environmental factors, or it might just be the luck of the draw. More research is needed.
Idiopathic scoliosis usually develops during growth spurts, so the most common age of onset is during puberty.
Boys and girls are both diagnosed at approximately the same rate.
However, female patients have a 10 times higher risk of the condition degenerating as they get older.
We have written an article about genes and what part they play in causing lower back pain here.
Minor cases generally only require monitoring, to ensure the condition is not getting worse.
The larger the angle of the spinal curve, the higher the odds that it will worsen over time.
As a result, idiopathic scoliosis is a lifetime concern, since it requires regular checkups.
Treatment for idiopathic scoliosis includes wearing a brace, physical therapy, and surgery in the most severe cases.
Congenital Scoliosis
Congenital scoliosis develops while a fetus is still growing inside of its mother.
Vertebrae may grow with a curved shape, or may not fully separate, leading to fused vertebrae.
Vertebrae may even be fused along one side, in a condition called “unilaterally fused vertebrae”, causing the spine to curve.
Depending on how severe the curvature is, doctors may identify the condition when the baby is delivered, or it may go unnoticed until later in life.
When identified early, congenital scoliosis may be entirely cured by applying a cast to correct the curvature.
Neuromuscular Scoliosis
Neuromuscular scoliosis develops as a secondary condition, due to another disease or medical condition.
These conditions can either cause bone degeneration or can cause the muscles and connective tissue around the spine to stop supporting it.
Here are a few of the conditions that can cause neuromuscular scoliosis:
- Muscular dystrophy. In this condition, muscles lose their strength. When the muscles around the spine weaken, especially if they weaken only on one side, spinal curvature can result.
- Birth defects. Birth defects like spina bifida can cause a baby’s vertebrae to develop abnormally. This is also a type of congenital scoliosis.
- Injuries or infections. Traumatic injury or serious infection can cause the spine to develop a curve.
- One leg is longer than the other. If one of your legs is longer than the other, you may lean to one side to compensate. Over time, this can develop into a permanent spinal curve.
- Cerebral palsy. Not all cases of cerebral palsy result in scoliosis. However, it does result in a handful of cases.
Scoliosis in Adults
Adult scoliosis is different than scoliosis in children or infants.
This is because an adult’s bones are already mature, so the treatment options may be different. Generally, adult scoliosis comes in three different types.
- First, adults who received surgery as adolescents may suffer from a relapse. When this occurs, a doctor may recommend a follow-up surgery or other treatment.
- Second, adults who developed scoliosis as adolescents, but did not receive surgery. When the condition progresses to the point where it causes pain, discomfort, or more severe symptoms, surgery or a brace may be required.
- Finally, it’s possible for adults to develop a condition called “degenerative scoliosis”, or “de novo scoliosis”. “De novo” means “new”, because the condition did not exist earlier in life. This type of scoliosis generally occurs in the lower back and mostly affects senior citizens. Degenerative scoliosis occurs as a result of the loss of bone and muscle strength due to aging. As a person’s muscles weaken and they lose bone density, the spine will naturally compress slightly. Normally, this happens evenly on both sides, which is why people get slightly shorter as they get older. However, sometimes the spine will compress more on one side than on the other side, leading to a curved shape. Degenerative scoliosis often causes spinal stenosis, which means that the spinal canal gets narrower and pinches spinal nerves. This can cause pain and discomfort, especially during physical activity. Because degenerative scoliosis only causes minor curving, surgery is generally not required. A normal course of treatment will involve pain management through medication and physical therapy.