Table of Contents
A herniated disc is a condition where one of the soft, rubbery discs between your vertebrae starts to bulge outwards.
The illustration below gives you a good (simplified) example of what is typical for a herniated disc.
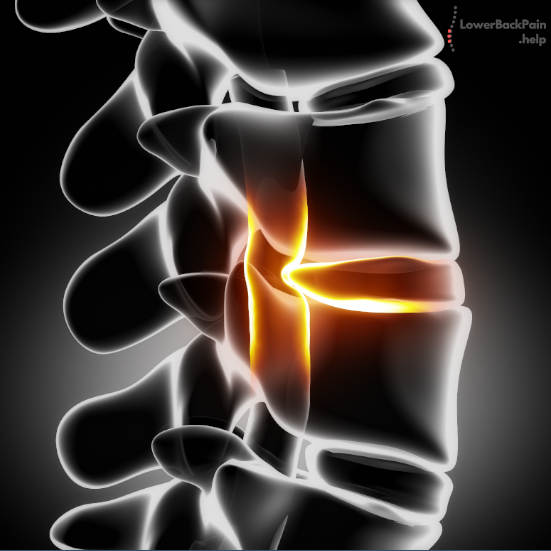
When these discs are in place and intact, they provide shock absorption and prevent vertebrae from rubbing against each other and pinching your nerves.
But when one of these discs herniates, it can press on nearby nerves. You find more in our article “what is a herniated disc?”
This can cause pain, tingling, numbness, or weakness in one of your limbs.
So, what’s the best treatment for a herniated disc?
First, we’ll talk about managing the pain that can come from a herniated disc.
Then, we’ll discuss reasons for concern, and when you might want to look for medical intervention.
Managing Herniated Disc Pain
Of course, the worst symptom of a herniated disc is the associated pain.
But how can you manage it?
Here are five proven methods that work for most herniated disc patients to ease the pain.
1) Hot and Cold Therapy
As with many physical issues, applying a hot or cold pad can help alleviate muscle pain and tension. Because the pain is ultimately in your muscles, not in the disc itself, this can be an effective solution – at least to give you temporary relief.
Heat therapy loosens muscle tension, which can help alleviate spasms.
It also increases blood flow and the elasticity of muscles, tendons, and ligaments.
Using a heating pad several times a day can significantly relieve many symptoms of a herniated disc.
When you do this, make sure to use a towel or paper towel to avoid burning yourself.
Heat therapy is ideal before workouts or combined with a stretching routine first thing in the morning.
And you don’t need a heating pad to apply heat. A warm bath or a hot shower can do wonders at the end of a long day’s work.
Cold therapy, on the other hand, reduces blood flow, which can reduce inflammation.
It also has a pain-relieving effect, in and of itself.
Cold therapy is ideal after workouts or physical activity since those are the times when inflammation is most likely to be an issue.
If you unsure if Hot or Cold Therapy is right for you please read our article that goes into more detail: Ice or Heat for Lower Back Pain. What you should use.
2) Light Exercise
You might think that exercise would be a bad idea for someone with a herniated disc.
However, light physical activity can provide several benefits. Primarily, exercise causes your body to release endorphins, which alleviate pain and improve your mood.
Ideal exercises for people with herniated discs include:
- Walking, either on a treadmill or outdoors
- Riding a stationary or recumbent bicycle
- Using an elliptical machine
- Swimming
As you can see, these are all low-impact exercises, which put minimal strain on your back.
If your pain is too severe for any of these exercises, consider swimming or hydrotherapy.
These activities place no stress whatsoever on your spine, so you don’t have to worry about your pain getting worse.
If you’re not sure what to try, it’s always a good idea to talk with your doctor.
3) Adjust Your Sleeping Position
One of the toughest things about living with a herniated disc is getting a good night’s sleep.
Thankfully, there are easy, affordable ways to fall and stay asleep.
Your exact best position is going to depend on where your herniated disc is located, so there isn’t a one-size-fits-all solution. However, we can still give you a couple of pointers:
- If your herniated disc is located in your lower back, try sleeping on your side with a pillow between your knees. For extra support, throw a second pillow under your abdomen.
- If the problem is in your upper back, try sleeping on your stomach. Put a pillow under your stomach to keep your spine as straight as possible.
We have written a whole article about Sleeping with Lower Back Pain where you can find more details.
4) Consider Physical Therapy
Physical therapy can provide major benefits to most people with herniated discs.
One popular method is the McKenzie Method, which involves a combination of stretches and low-impact exercises.
Once that has been achieved, the next phase involves long-term rehab, strengthening your back muscles, and managing your back pain.
Even after the herniated disc has healed, continued physical therapy can keep your back muscles strong and supple, reducing the risk of re-injury.
If you google for the McKenzie Method you will find lots of good and reliable information on how to get started.
5) Massage or Myofascial Release
Myofascial tissue is the tough, sinewy tissue that wraps around all your muscles and supports them.
This tissue can be a major source of pain when you have a herniated disc.
Myofascial release therapy is designed to relax these tissues, particularly around “trigger points” where the muscles connect to tendons.
It generally takes place in the context of massage therapy or physical therapy session.
Massage therapy, in general, can also be incredibly helpful.
By relaxing your muscles, you give your disc and connective tissues relief from pressure, which gives them time to heal.
Even a massage chair or home massage tool can provide a lot of relief.
A visit to the Chiropractic is also a great help and one of the best treatments for a herniated disc. While it won’t fix the disc itself, it will help with general spinal alignment and relaxation.
To cheer you up if you are in pain from a herniated disc at this moment: most herniated disc pain will clear up in about 6 weeks.
Do I Need Surgery?
Generally, surgery is not necessary to treat a herniated disc in the vast majority of cases.
The risks of complications are relatively high, and the effectiveness is limited.
However, there are a few symptoms that can justify surgical intervention, particularly if they continue for more than a few months.
These include:
- Continued numbness or weakness
- Continued severe pain
- Difficulty standing, walking, or performing everyday tasks
- Bladder or bowel incontinence
In most cases, a surgeon will be able to remove only the bulging portion of the disc.
However, as we said, surgery has its risks.
In some cases, the entire disc will need to be removed, and your vertebrae may even need to be fused. This requires the insertion of metal hardware and several months of recovery.
In short, while surgery is sometimes necessary, it’s best to avoid it whenever possible.
