Table of Contents
Many people with back pain may be concerned that they have a herniated disc or may be told by a medical professional that this might be the case.
But what exactly are herniated discs, and how can you know if you have one?
How Does a Herniated Disc Occur?
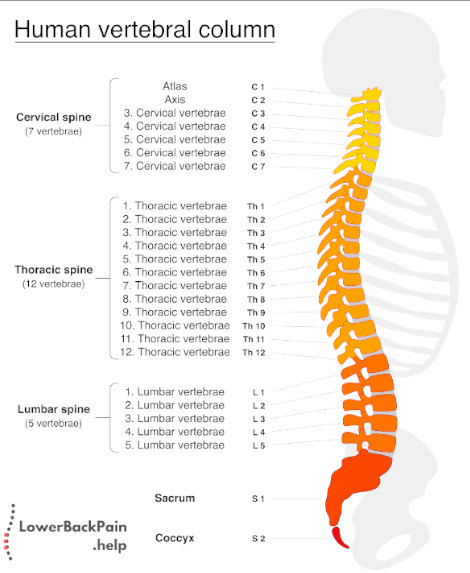
The human spine is made up of a long series of interconnected bones called vertebrae. Each of these interlocking bone pieces is cushioned by separate discs. These are normally round and soft like pillows with a tougher outer layer that surrounds the softer interior of the disc. In this way, the discs perform a critical function and acted like shock absorbers for your vertebrae.
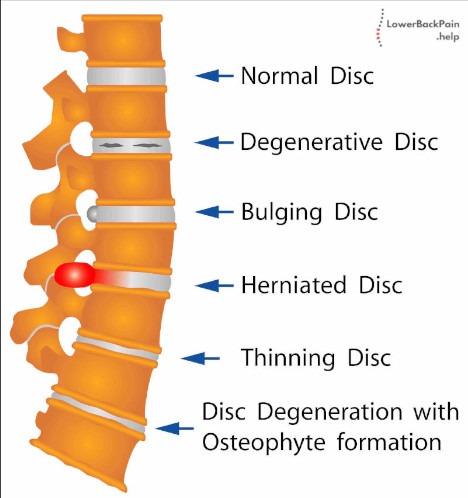
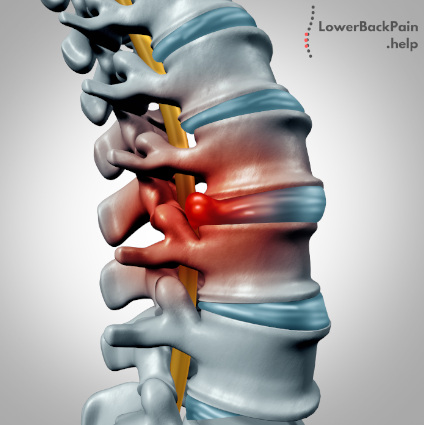
Herniated discs, which can also be called ruptured, slipped, or bulged, are discs that are moved out of proper position. Specifically, a fragment of the hernia disc is pushed out of the tougher layer and into the spinal canal. This usually occurs if the hernia disc’s outer layer is ruptured or torn from injury or a particular movement. The image below shows different conditions that can happen to the discs.
The human spine is relatively compact and tight, which means that any herniated disc stands a good chance of pressing on spinal nerves.
The spine is the focal point for the entire human nervous system, meaning that a minor injury here can lead to pain throughout the body.
Where Do Herniated Discs Happen?
Herniated discs can occur anywhere along your spine, although they are more common along the lower or lumbar area. Another frequent spot is near the neck, called the cervical spine.
The exact area in which you experience a herniated disc can dictate the kind of discomfort or pain you feel.
What Causes Herniated Discs?
Herniated discs can be caused by several potential reasons.
While the spine is made to be flexible, it’s also fragile in its own way.
A single bad movement for an excessive tug in the wrong direction can lead to a herniated disc. This is why many people who perform intense manual labor end up experiencing a herniated disc at one point or another.
However, the material around spinal discs naturally degenerates as we get older.
The ligaments that hold spinal discs in place we can over time, which makes it easier to rupture the disc from normal movement or wear and tear.
Finally, those with genetic predispositions for weak discs or spinal tissue may also experience an increase in herniated discs relative to the general population.
There has been some research showing that some family lines have genes that predispose individuals to herniated discs.
How to Tell if You Have a Herniated Disc
How do you tell if you have a herniated disc? Your symptoms can vary greatly, especially depending on where the herniated disc is and how intense the rupture is.
There are some rare instances in which the herniated disc doesn’t press on any other nerve, which means pain is relatively minor. Such individuals may only experience a very mild backache or not feel any discomfort at all.
Much more common is that most of the pain comes from the disc pressing on nerves in the surrounding area.
In addition, herniated discs usually give you lots of warning, either by causing intermittent periods of low back pain or a single drawn-out ache that lasts for several weeks.
Sciatica, which is intense pain affecting the sciatic nerve along the lower back and down your legs, is another big sign of a herniated disc. That’s because sciatica is often caused by such a disc pressing on the nerve, which is one of the largest and is the longest in your body.
Cervical pain around your neck, either dull or sharp, may also be a sign of a herniated disc near your neck. This pain will typically radiate down your arms and may be accompanied by tingling in your shoulders. You may feel more intense pain as you move your neck from side to side or in different places.
Treatments for Herniated Discs
If you think you have a herniated disc, there’s no need to instantly worry about surgery; most herniated discs require none.
In general, people with herniated discs find relief within a few weeks.
Home remedies, in general, include limiting your activities and range of motion for a few days.
You should go to a doctor regardless, as they’ll be able to identify whether a herniated disc is actually the cause of your lower back pain.
Your doctor may recommend medicine for the pain.
You can most likely be a little bit more active once you have taken the pain medication for some days.
Getting active again is important.
It will support you to get fitter.
However, your doctor might recommend staying in bed and rest for a longer period if your pain is severe.
Your doctor likely won’t use an MRI unless your symptoms have been present for a much longer period than a few weeks.
A doctor may also recommend physical therapy, which may include certain types of massage or stretching or therapy with hot or cold patches and pouches. More advanced potential remedies include using ultrasound therapy, electrical muscle stimulation, and even steroid injection to the local disturbed area.
Only in the most extreme cases will your doctor refer you to a spine specialist or a neurosurgeon.
This may lead to surgery to repair disc damage or realign the spine, although these cases are relatively rare compared to all who experience a herniated disc.
You should only expect the need for surgery if you have significant weakness in the arms and legs or you begin to lose your feeling in certain areas of your body, like your genitals or rectum.
Conclusion
If you think you have a herniated disc, see your doctor as soon as possible and let them give you a professional recommendation.
Be honest about the level of pain you’re experiencing, as this will determine the kind of treatment you are best suited for.
Take some comfort in the fact that your herniated disc is likely not a major issue and will probably be treated within a few weeks – even when the pain can be severe.
